Blog
Jan 15, 2026
What Your Flagged Vitals Mean
Heart rate elevated. Temperature flagged. Here's what your body is actually telling you.

Your wrist temperature is elevated. Your heart rate is higher than usual. Your respiratory rate changed overnight.
You see the flag. You check the number. And then... nothing. The data tells you what shifted, but not why it matters or whether you should actually do anything about it.
If you track overnight vitals with Peaks, your Apple Watch, Oura Ring, or similar device, you've been here. A metric gets flagged as outside your typical range. You wonder if you're getting sick, if last night's dinner was too late, or if your body is just having an off night. The tracking tells you something changed. It doesn't tell you what that change means.
This is the interpretation gap. Your device measures with precision. It establishes your baseline over time. It flags deviations. But it stops short of explaining whether a flagged vital is your body fighting off illness, reacting to that glass of wine, or just normal noise you should ignore.
Here's how to read each vital when it gets flagged, what actually causes the changes, and when a flagged number deserves your attention.
Heart Rate: Your Overnight Stress Indicator
Your heart rate during sleep typically drops 20-30% below your waking resting rate. For most healthy adults, that means somewhere between 40-60 beats per minute, though athletes can go lower and less conditioned individuals may sit higher in the 60-100 range.
When your overnight heart rate gets flagged as elevated, your body is working harder than usual while you sleep. This happens for several specific reasons, and most of them aren't medical emergencies.
Late eating creates the most common false alarm. When you eat close to bedtime, your digestive system stays active overnight. Blood flow increases to your stomach and intestines. Your heart rate stays elevated to support digestion instead of dropping into its typical recovery pattern. Research on sleeping heart rate patterns shows this creates a "downward slope" instead of the ideal "hammock curve" where your heart rate bottoms out mid-sleep.
Alcohol raises overnight heart rate reliably. Even one drink increases your heart rate during sleep as your body metabolizes the alcohol. This effect is dose-dependent—more drinks mean a higher, more sustained elevation. If you see a flagged heart rate after drinking, that's expected physiology, not a health concern.
Stress and anxiety keep your heart rate elevated through the night. Your sympathetic nervous system ("fight or flight") stays more active when you're stressed, preventing the normal parasympathetic dominance that allows heart rate to drop during sleep. If you had a stressful day or went to bed anxious, elevated overnight heart rate is your nervous system's way of staying on guard.
Illness brewing often shows up in heart rate first. Your body increases circulation to support your immune response before you feel symptomatic. Multiple studies have found that elevated overnight heart rate can precede cold and flu symptoms by 1-3 days. If your heart rate is flagged and stays elevated for multiple nights without an obvious lifestyle cause, pay attention to how you feel. Your body may be fighting something.
Exercise timing matters too. Intense workouts close to bedtime can keep your heart rate elevated for hours afterward. Your body's recovery processes—clearing lactate, replenishing glycogen, repairing muscle—all require increased circulation.
When your overnight heart rate is flagged as unusually low, the interpretation flips. For most people, a lower-than-usual heart rate signals excellent recovery. Your parasympathetic nervous system is dominant, your body is deeply relaxed, and you're getting restorative sleep. Athletes in particular see this after adaptation to training.
However, a very low heart rate (below 40-50 bpm for non-athletes) accompanied by dizziness, fatigue, or feeling unwell could indicate a medical issue or medication effect. Beta-blockers and some other medications deliberately lower heart rate. If you're not on these medications and your heart rate drops significantly below your baseline with symptoms, that warrants a conversation with your doctor.
What to do when heart rate is flagged:
Single night elevated, no symptoms → Review yesterday's behavior (late meal? alcohol? stress? hard workout?)
Multiple nights elevated, feeling fine → Probably lifestyle pattern, try adjusting habits
Multiple nights elevated + feeling off → Your body might be fighting illness, take it easy
Unusually low with symptoms → Check with your doctor
Unusually low without symptoms → You're probably just very well-recovered
Wrist Temperature: The Lifestyle Detective
Your wrist temperature while sleeping follows a predictable pattern. It rises as you fall asleep, plateaus during the night, then drops sharply when you wake. Over the course of sleep, your wrist stays warmer than during the day—the opposite of your core body temperature, which drops overnight.
Normal variations in wrist temperature can range up to 1.8°F (1°C) from one night to another. This makes temperature one of the more sensitive vitals, frequently flagged even when nothing is particularly wrong.
Alcohol is the most reliable temperature elevator. Peripheral vasodilation (blood vessels near your skin expanding) increases blood flow to your extremities, raising skin temperature at your wrist. This effect is so consistent that researchers studying wrist temperature specifically note alcohol as a primary confounding variable. If your temperature is flagged after drinking, that's pharmacology, not pathology.
Room temperature and bedding affect wrist temperature directly. Unlike core body temperature, which your body regulates tightly, peripheral skin temperature responds to your environment. A warm room, heavy blankets, or sleeping on your wrist can all raise the temperature your device measures. Before assuming something is wrong with your body, consider your sleep environment.
Menstrual cycles create predictable temperature patterns. During the luteal phase (after ovulation), body temperature—including wrist temperature—rises and stays elevated until menstruation. Research comparing wrist skin temperature to basal body temperature shows wrist measurements are more sensitive to these hormonal shifts, with temperature increases of 0.5°C or more. If you track your cycle, elevated wrist temperature during this phase is expected.
Illness raises temperature, but not always immediately. Fever shows up in wrist temperature, but subclinical immune responses (your body fighting infection before you have a measurable fever) can also cause mild elevations. Data from Apple Watch users shows wrist temperature often elevates 1-3 days before people feel sick, similar to heart rate.
Lower-than-usual wrist temperature is less common but can happen. Cold sleeping environments are the usual cause. Some people see decreased temperature with dehydration or poor circulation. If your wrist temperature is consistently lower than your baseline and you feel cold or notice circulation changes, mention it to your doctor. Otherwise, a single low reading is likely environmental.
What to do when wrist temperature is flagged:
Elevated after alcohol → Expected, ignore
Elevated mid-cycle (women) → Likely hormonal, normal
Elevated with warm room/heavy blankets → Environmental, adjust sleep setup
Elevated 2-3 nights + other flagged vitals → Possible illness brewing, monitor symptoms
Unusually low → Check room temperature first, consider hydration
Respiratory Rate: The Congestion and Recovery Signal
Your respiratory rate during sleep should be lower and more stable than during the day. Normal sleeping respiratory rate for adults ranges from 12-20 breaths per minute, often settling toward the lower end during deep sleep when your body's oxygen demands decrease.
Elevated respiratory rate has fewer benign causes than heart rate or temperature. When this vital gets flagged, it usually means something is actually happening.
Congestion and respiratory infections increase breathing rate overnight. When your airways are partially obstructed—from a cold, allergies, or sinus congestion—your body compensates by breathing more frequently to maintain oxygen levels. This is often one of the first vitals to flag when you're getting sick, sometimes before you notice the congestion yourself.
Anxiety and stress can elevate respiratory rate during sleep. Similar to heart rate, your sympathetic nervous system activation keeps breathing rate higher than baseline. People with anxiety disorders or those under significant stress often see elevated overnight respiratory rate alongside elevated heart rate.
Sleep apnea causes complex respiratory patterns that may or may not flag as elevated on average, depending on how your device calculates the metric. If you consistently see elevated respiratory rate alongside poor sleep quality, wake feeling unrested despite adequate time in bed, or have a partner who reports you snore or stop breathing, sleep apnea screening is worth pursuing.
Lower-than-usual respiratory rate typically indicates deep, efficient sleep and strong recovery. Your body needs less oxygen during rest, so breathing slows. Athletes and very fit individuals often see lower overnight respiratory rates. This is generally a positive sign.
What to do when respiratory rate is flagged:
Elevated with nasal congestion → You're stuffed up, treat the congestion
Elevated with no obvious cause → Monitor for illness developing
Elevated alongside elevated heart rate → Stress, illness, or both
Consistently elevated + poor sleep quality → Consider sleep apnea screening
Lower than usual → Good recovery, you're doing well
Blood Oxygen: The Altitude and Airway Vital
Blood oxygen during sleep should stay above 95% for most healthy adults. Your device measures oxygen saturation (SpO2)—the percentage of hemoglobin in your blood that's carrying oxygen.
Altitude is the most common reason for flagged oxygen levels in healthy people. As elevation increases, the partial pressure of oxygen in the air decreases. Your body compensates, but overnight SpO2 often drops at altitude, especially in the first few nights before acclimatization. If you recently traveled to a higher elevation or are visiting somewhere mountainous, lower oxygen readings are expected.
Sleep apnea causes repeated oxygen desaturations overnight. Unlike the gradual, sustained drop from altitude, sleep apnea creates a pattern of dips and recoveries as breathing stops and restarts. If your oxygen is frequently flagged alongside poor sleep quality, loud snoring, or daytime fatigue, sleep apnea evaluation is important. This is one of the few vital changes that warrants medical attention rather than lifestyle adjustment.
Congestion from colds, allergies, or sinus issues can mildly reduce oxygen saturation by limiting airflow. This usually resolves when the congestion clears.
Some devices show more oxygen variability than others. Wrist-worn devices measure SpO2 optically, which is less precise than medical-grade pulse oximetry. Small movements, poor sensor contact, or cold extremities can create measurement artifacts. A single low reading without symptoms is often measurement noise rather than true hypoxemia.
What to do when blood oxygen is flagged:
Recently traveled to altitude → Normal, monitor for acclimatization
Congested from cold/allergies → Likely related, should improve as congestion clears
Consistently low + snoring/poor sleep → Pursue sleep apnea screening
Single isolated reading → Probably measurement error, ignore unless repeated
Persistent low readings → See a doctor
When One Flagged Vital Matters (And When It Doesn't)
The pattern matters more than any single data point.
One night, one flagged vital, no symptoms: Ignore it. You probably had a glass of wine, ate late, slept warm, or your device caught measurement noise. Your body has normal night-to-night variation. Single deviations are usually lifestyle factors or environmental effects.
One night, multiple flagged vitals, no symptoms: Pay attention. When heart rate, temperature, and respiratory rate all flag together, your body is reacting to something—often illness brewing that you can't feel yet. Studies tracking Apple Watch Vitals users found that multi-vital flags preceded symptomatic illness by 1-3 days in many cases. Take it easy, hydrate, skip the hard workout.
Multiple consecutive nights, same vital flagged, no symptoms: Look for a pattern. Did your habits change? New medication? Different sleep environment? Sleep schedule shift? If you identify the cause, you can decide whether to adjust it. If nothing obvious changed and you feel fine, monitor but don't panic.
Multiple consecutive nights, same vital flagged, with symptoms: Trust your body. The data is confirming what you feel. You're actually sick, actually stressed, actually not recovering. This is when tracking vitals proves useful—it validates that something is off and helps you track recovery as the numbers return to baseline.
Any flagged vital with concerning symptoms: See a doctor. If you have chest pain, severe shortness of breath, extreme fatigue, persistent fever, or anything else that worries you, the vital signs are secondary to the symptoms. The tracking is helpful context to share with your healthcare provider, but symptoms trump data.
The goal of tracking overnight vitals isn't to create health anxiety over every flagged number. It's to give you earlier signals than you'd notice otherwise and help you distinguish lifestyle noise from meaningful changes. Most flagged vitals are your body reacting to your behavior—late meals, alcohol, stress, exercise timing, sleep environment. When you spot these patterns, you can adjust your habits and see your vitals stabilize.
The vitals that matter are the ones that persist across multiple nights or align with how you actually feel. A single elevated heart rate after pizza at 10pm is information, not an emergency. An elevated heart rate three nights running before you develop a fever is useful warning. Learning to tell the difference turns raw data into actual insight about your health.

What's Actually Happening While You Sleep
Your brain cycles through distinct stages every night, each with a specific job. Understanding them explains why some nights leave you restored and others don't.

The Sleep You're Missing Is Adding Up
You've adjusted to feeling tired. But your body is keeping a running tab, and it's not as easy to pay off as you think.
4.7 1.100+ Reviews
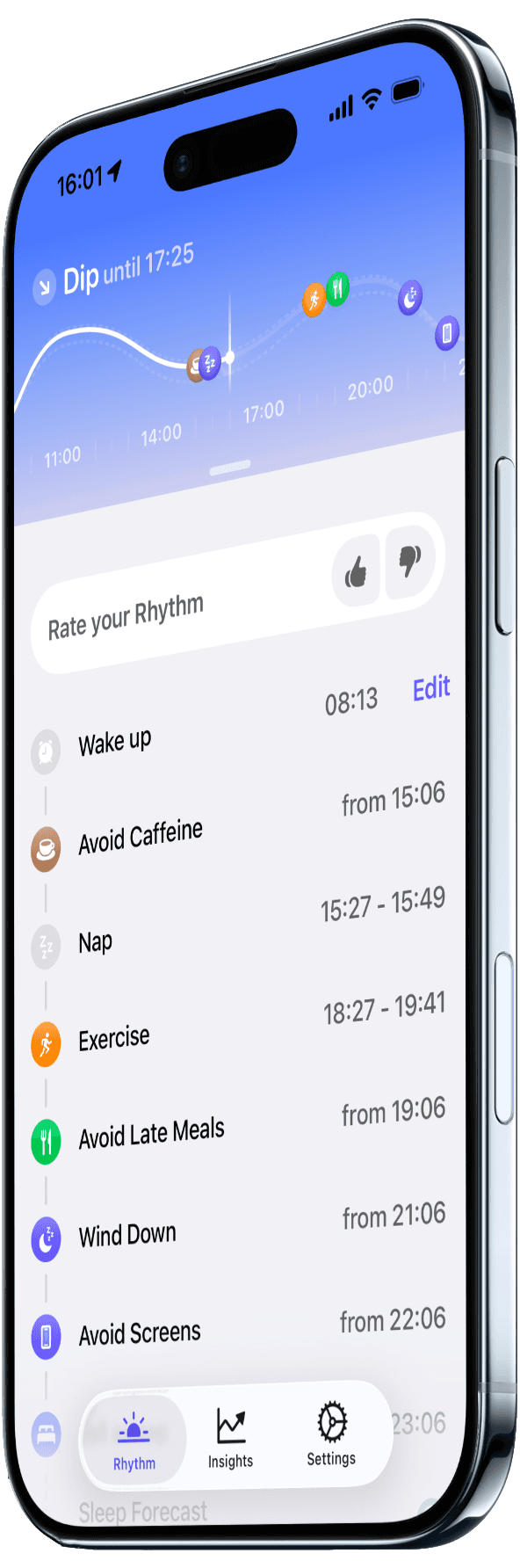
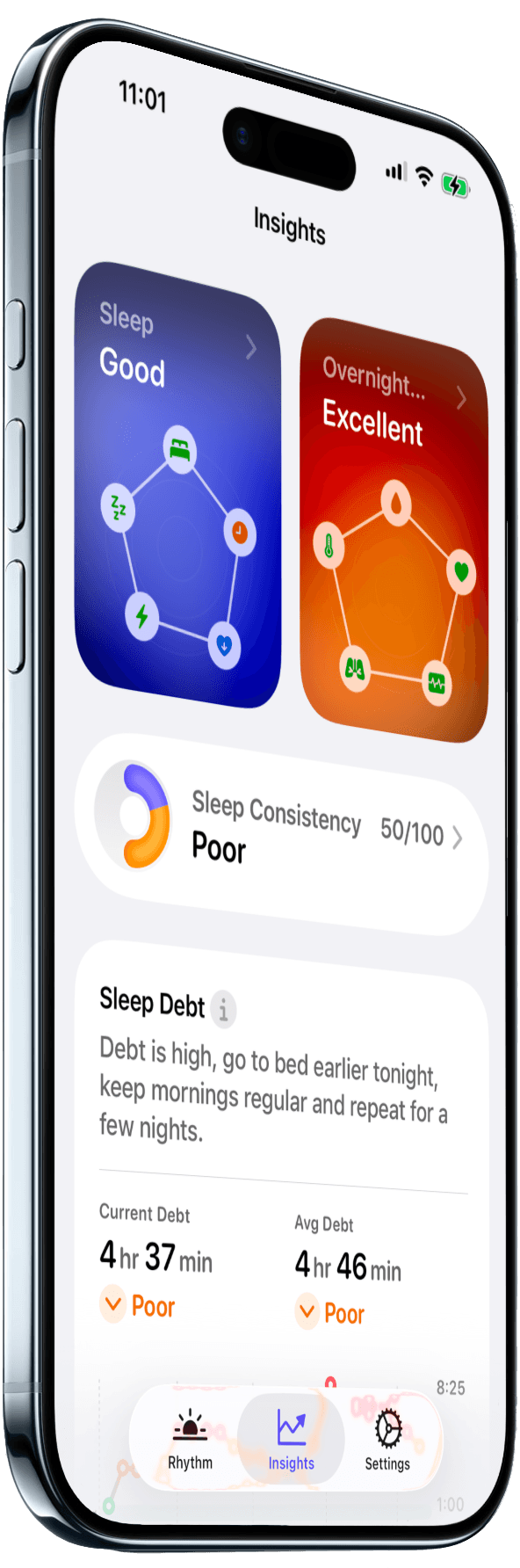
Track What Your Body Does While You Sleep
Peaks displays your overnight vitals from Apple Watch, helping you spot the patterns that matter.